Protocol - Body Proportions
- Arm Span
- Current Age
- Height - Knee Height
- Height - Recumbent Length
- Height - Self-Reported Height
- Height - Standing Height
- Weight - Measured Weight
- Weight - Self-Reported Weight
Description
The arm span to height comparison is determined by measuring the individual’s arm span and standing height and then comparing the two measurements (e.g., arm span is 3 centimeters greater than height). The upper to lower body segment ratio is a physical measurement of an individual’s upper segment versus lower body segment and expressed as a ratio (e.g., 1.2:1).
Specific Instructions
These characteristics may apply to Marfan syndrome, homocystinuria, Klinefelter syndrome, and all skeletal dysplasias such as spondyloepiphyseal dysplasia, and achondroplasia.
All measurements are based on the individual’s age and may differ by sex, race, and ethnicity.
The notion of recommending replicate measurements comes from the reduction in random errors of measurement and accompanying improved measurement reliability when the mean of multiple measurements is used rather than the a single measurement. This improvement in measurement reliability, however, depends upon the reliability of a single measurement in the hands of the data collectors in a particular study (Himes, 1989). For example, if a measure like recumbent length in a given study has a measurement reliability of 0.95 (expressed as an intraclass correlation coefficient), taking a second measurement and using the mean of the two in analyses will only improve the reliability to 0.97, yielding only a 2% reduction in error variance for the additional effort. If in the same study the reliability of a single triceps skinfold measurement was 0.85, using the mean including a replicate measurement would raise the reliability to 0.92 and yield a 7% reduction in error variance, more than a threefold better improvement compared with recumbent length. The intraclass correlation coefficient is specifically recommended here for assessing reliability because it takes account of both random and systematic errors of measurement, whereas the interclass correlation (e.g., Pearson correlation) takes account of only random errors of measurement.
Because the benefits of taking replicate measurements are so closely linked with the existing measurement reliability, it is recommended that as a part of the training of those who will be collecting anthropometry data, a reliability study be conducted that will yield measurement reliability estimates for the data collectors, protocols, settings and participants involved in that particular study (Himes, 1989). If the measurement reliability for a single measurement ≥ 0.95 the recommendation is that replicate measurements are not necessary and will yield little practical benefit. If the measurement reliability <0.95 the recommendation is to include replicate measurements as prescribed.
If replicate measurements are indicated because of relatively low reliability, a second measurement should be taken, including repositioning the participant. A third measurement should be taken if the first two measurements differ by >0.5 cm. If it is necessary to take a third measurement, the two closest measurements are averaged. Should the third measurement fall equally between the first two measurements, all three should be averaged.
Availability
This protocol is freely available; permission not required for use.
Protocol
Arm span to height comparison: Measure the arm span of the individual per the Arm Span protocol, which appears below. Measure standing height per the protocol for Standing Height, which also is below. Record measurements to the nearest 0.1 centimeter. Normally the arm span is less than the height in boys up to 10 years of age and in girls up to 11 years of age. The arm span is approximately 5 cm greater than the height in adult males and 1.2 cm in adult females. Arm span that is significantly greater than the height should be investigated further for disproportionate growth. Some conditions such as spondyloepiphyseal dysplasia and scoliosis, may be associated with a disproportionately short trunk. Excessively long arms may be indicative of Marfan syndrome, Klinfelter syndrome, or homocystinuria.
Upper to lower body segment ratio: The individual should stand straight with his/her back against a flat wall. With a flexible measuring tape, measure from the upper border of the symphysis pubis to the floor*, to the nearest 0.1 centimeter. Record this measurement as the lower segment. Measure the standing height per the protocol for Standing Height. Subtract the lower segment from the standing height for the upper segment measurement. The upper segment measurement over the lower segment is the ratio. The typical ratio is 1.7:1 at birth and decreases by 0.1 cm for every year of age. At 10 years of age, the ratio becomes 1:1 and remains so. In conditions such as congenital hypothyroidism, the upper segment remains disproportionately longer.
*If it is difficult to locate the symphysis pubis, the sitting height should be measured (see protocol for Sitting Height below). The sitting height measurement can be subtracted from the standing height measurement to determine the value for the lower segment.
Arm Span
This protocol is part of an examination survey. It requires a tape measure at least 2 m long, a flat surface (usually a wall), and an adjustable block that is fixed to the wall. The spool of the tape measure is fixed to the adjustable block. The block serves as the contact point for the middle (longest) finger of the right hand, which is in contact with the block when the participant is positioned. The block must be movable so that it can be adjusted vertically to accommodate individuals of varying stature. The block is adjusted to bring the tape to the shoulder level for the subject, and then the tape is pulled horizontally along the wall. The participant stands with the feet together so that his or her back is against the wall. The arms are outstretched laterally and maximally at the level of the shoulders, in contact with the wall, and with the palms facing forward. The tip of the middle (longest) finger (excluding the fingernail) of the right hand is kept in contact with the block, while the zero end of the tape is set at the tip of the middle (longest) finger (excluding the fingernail) of the left hand. Two people (measurers) are necessary, one at the zero end of the tape to be sure the tape end is positioned correctly and the other at the block end to make the reading. The measurement is recorded to the nearest 0.1 cm. Occasionally, a small stool may be required for the measurers to make this measurement on tall subjects (when the measurer is shorter than the study subject). When making this measurement, it is imperative that the participant’s arms be outstretched maximally and that they are held in this position until the reading is taken. Special care must be taken with young children and older individuals as they tend to lower their arms during the measurement.
Standing Height
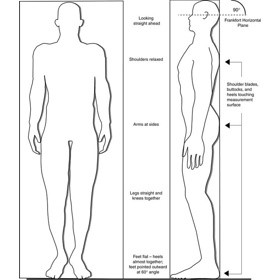
Ask the participant to remove hair ornaments, jewelry, buns, or braids from the top of the head that interfere with the measurement. Shoes should be removed. Ask the participant to stand erect against the backboard with the body weight evenly distributed and both feet flat on the stadiometer platform (Exhibit 1). The participant’s feet should be positioned with the heels together and toes pointed slightly outward at approximately a 60 degree angle. Check to be sure that the back of the head, shoulder blades, buttocks, and heels make contact with the backboard of the stadiometer. NOTE: Depending on the overall body conformation of the individual, all four contact points - head, shoulders, buttocks, and heels - may or may not touch the stadiometer backboard (Exhibit 2). For example, elderly survey participants may have kyphosis, a forward curvature of the spine that appears as a hump at the upper back. In particular, dowager’s hump is a form of kyphosis that creates a hump at the back of the neck. Additionally, some overweight survey participants cannot stand straight while touching all four contact points to the backboard. In such instances it is important to obtain the best measurement possible according to the protocol. Stature measurements are made with the head aligned in the Frankfort horizontal plane (Exhibit 2). The head is in the Frankfort plane when the horizontal line from the ear canal to the lower border of the orbit of the eye is parallel to the floor and perpendicular to the vertical backboard (see Exhibit 2). Many people will assume this position naturally, but for some survey participants, the examiner may need to gently tilt the head up or down to achieve the proper alignment. Instruct the survey participant to look straight ahead. If you cannot position the participant such that his or her trunk remains vertical above the waist, that the arms and shoulders are relaxed, and that the head is positioned in the Frankfort plane, be sure to note this in the measurement record. This information might be useful to interpret study findings. In the National Health and Nutrition Examination Study 2007-08, a comment described as "Not Straight" is noted in the stature record. Once positioned, lower the stadiometer headpiece so that it rests firmly on top of the participant’s head, with sufficient pressure to compress the hair. Instruct the survey participant to stand as tall as possible, take a deep breath, and hold this position. The act of taking a deep breath helps straighten the spine to yield a more consistent and reproducible stature measurement. Notice that the inhalation will cause the headpiece to rise slightly. As soon as the participant inhales, record the measurement. After recording the measurement, tell the participant to relax. Once the measurement is taken, raise the stadiometer headpiece and have the participant step away from the stadiometer. Adjustments for shoes and hair: When participants cannot remove hair braids, buns, and headwear that interferes with the stature measurement, measure the distance from the scalp to the top of the hair with a small ruler to the nearest 0.1 cm. If shoes are worn, measure the height of the shoe heel to the nearest 0.1 cm. A corrected height value can be calculated by subtracting these distances from the original stature measurement, thus yielding an adjusted stature value.
Exhibit 1. Stadiometer with a fixed-length backboard and an adjustable headpiece

Exhibit 2. Body orientation for standing height measurement and Frankfort Horizontal Plane
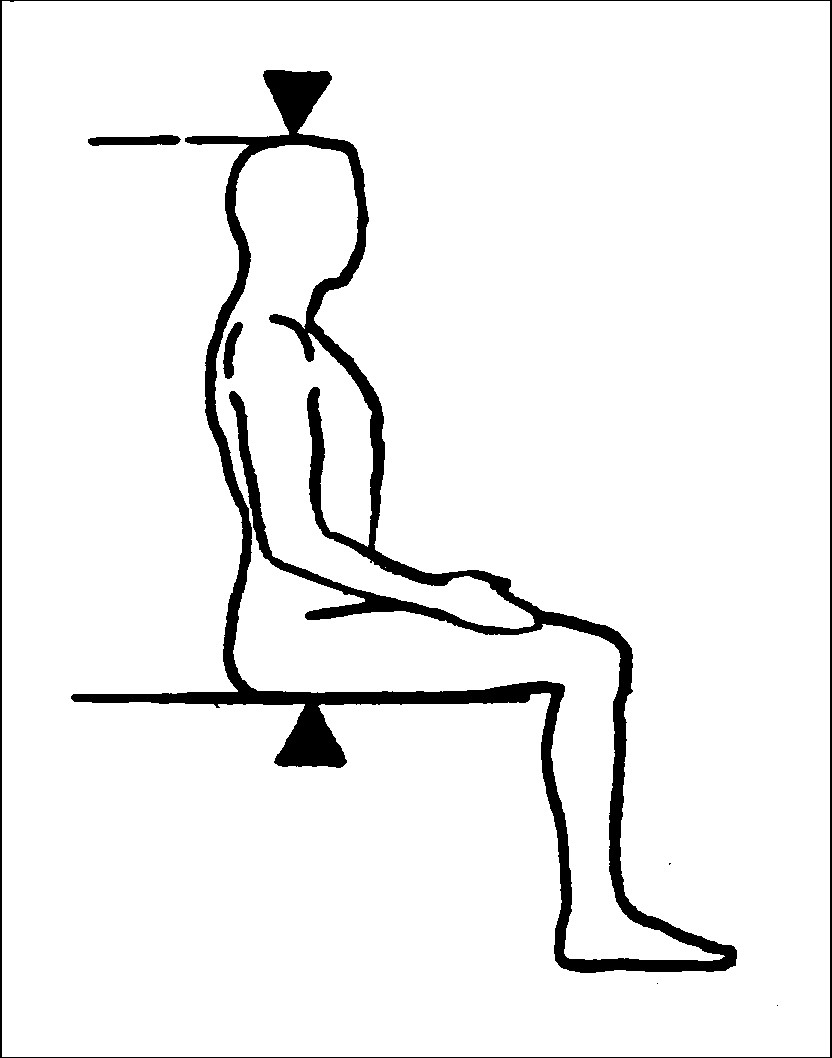
Sitting Height
For measuring sitting height, the examiner moves the specially made measurement box onto the floor board of the stadiometer. The participant then sits on the box with his or her back and buttocks to the backboard of the stadiometer. The participant sits as erect as possible with the head in the Frankfort Horizontal Plane position (see Exhibit 3). The knees are directed straight ahead with the arms and hands resting at the sides (see Exhibit 4). Ask the participant to sit tall and take a deep breath, and then lower the horizontal bar of the stadiometer down to the top of the head. The participant’s head is maintained in the Frankfort Horizontal Plane position throughout, and sufficient pressure is applied to the bar to compress the hair. Measurements will be recorded by the recorder to the nearest 0.1 cm.
Exhibit 3. Frankfort Horizontal Plane
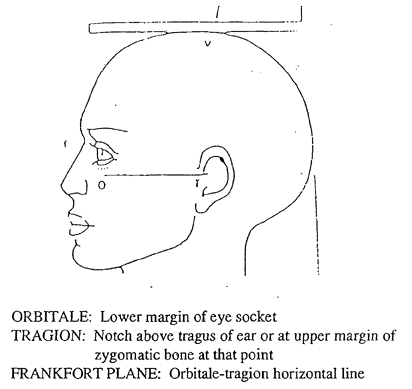
Exhibit 4. Participant position for Sitting Height
Personnel and Training Required
None
Equipment Needs
Flexible measuring tape
Requirements
| Requirement Category | Required |
|---|---|
| Major equipment | No |
| Specialized training | No |
| Specialized requirements for biospecimen collection | No |
| Average time of greater than 15 minutes in an unaffected individual | No |
Mode of Administration
Physical Measurement
Lifestage
Toddler, Child, Adolescent, Adult
Participants
Ages 1 or older
Selection Rationale
The Rare Genetic Conditions Working Group identified body proportions as a standard, simple, noninvasive method to determine the presence and location of disproportionate growth. Variations of growth are a common feature in rare genetic conditions, such as Marfan syndrome, Klinefelter syndrome, and achondroplasia.
Language
English
Standards
| Standard | Name | ID | Source |
|---|---|---|---|
| Human Phenotype Ontology | Limb undergrowth | HP:0009826 | HPO |
| caDSR Form | PhenX PX220201 - Body Proportions | 6200824 | caDSR Form |
| Logical Observation Identifiers Names and Codes (LOINC) | PhenX - body proportions protocol 220201 | 93000-8 | LOINC |
Derived Variables
None
Process and Review
Not applicable.
Protocol Name from Source
National Health and Nutrition Examination Survey (NHANES), Anthropometry procedures, 2007-2008
Source
Body Proportions
Lifshitz, F. (Ed.). (2007). Pediatric endocrinology, fifth Edition, volume 2: Pediatric endocrinology: Growth, adrenal, sexual, thyroid, calcium, and fluid balance disorders. New York, NY: Informa Healthcare USA.
Arm Span
Lohman, T. G., Roche, A. F., & Martorell, R. (Eds.). (1988). Anthropometric standardization reference manual. Champaign, IL: Human Kinetics.
Standing Height
Centers for Disease Control and Prevention. (2007). National Health and Nutrition Examination Survey 2007-2008 Anthropometry procedures manual. Retrieved from www.cdc.gov/nchs/data/nhanes/nhanes_07_08/manual_an.pdf
Sitting Height
Westat, Inc. (1988). National Health And Nutrition Examination Survey III: Body measurements (anthropometry). Prepared for the Centers for Disease Control and Prevention. Retrieved from
www.cdc.gov/nchs/data/nhanes/nhanes3/cdrom/nchs/manuals/anthro.pdf
General References
Chumlea, W. C., Guo, S. S., Wholihan, K., Cockram, D., Kuczmarski, R. J., & Johnson, C. L. (1998). Stature prediction equations for elderly non-Hispanic, white, non-Hispanic black, and Mexican American persons developed from NHANES III data. Journal of the American Dietetic Association, 98(2), 137-142.
Gripp, K. W., Slavotinek, A. M., Hall, J. G., & Allanson, J. E. (2013). Handbook of physical measurements (3rd ed.; Oxford Handbook Series). New York, NY: Oxford University Press.
Himes, J. H. (1989). Reliability of anthropometric methods and replicate measurements. American Journal of Physical Anthropology, 79(1), 77-80.
Nwoso, B., & Lee, M. (2008). Evaluation of short and tall stature in children. American Family Physician, 78(5), 597-604.
Protocol ID
220201
Variables
Export Variables| Variable Name | Variable ID | Variable Description | dbGaP Mapping | |
|---|---|---|---|---|
| PX220201_Body_Proportions_Arm_Span | ||||
| PX220201010000 | Measurement of the arm span | Variable Mapping | ||
| PX220201_Body_Proportions_Lower_Segment | ||||
| PX220201040000 | measurement from the upper border of the more | N/A | ||
| PX220201_Body_Proportions_Sitting_Height | ||||
| PX220201030000 | Measurement of the sitting height | Variable Mapping | ||
| PX220201_Body_Proportions_Standing_Height | ||||
| PX220201020000 | Measurement of the standing height | N/A | ||
| PX220201_Body_Proportions_Upper_Lower_Ratio | ||||
| PX220201060000 | Ratio of the upper segment measurement over more | N/A | ||
| PX220201_Body_Proportions_Upper_Segment | ||||
| PX220201050000 | measurement of the upper body segment by more | N/A | ||
Measure Name
Body Proportions
Release Date
April 30, 2015
Definition
Physical measures of an individual’s torso and extremities to determine if an individual has disproportionate growth.
Purpose
Disproportionate growth based on age is frequently used as criteria for many common or rare genetic diseases and conditions.
Keywords
Endocrine, growth, height, weight, Developmental Delay, Learning Disability, intellectual disability, intrauterine growth restriction, IUGR, childhood, toddler, adolescent
Measure Protocols
| Protocol ID | Protocol Name |
|---|---|
| 220201 | Body Proportions |