Protocol - Pediatric NIH Stroke Scale (PedNIHSS)
- History of Stroke - Ischemic Infarction and Hemorrhage
- Recovery and Recurrence Questionnaire (RRQ) - Pediatrics
- Stroke Impact Scale (SIS) - Adults
- Stroke Risk in Children with Sickle Cell Disease - TCD
- Stroke Risk in Children with Sickle Cell Disease - TCDi
Description
The Pediatric NIH Stroke Scale (PedNIHSS) is a physical assessment of the various symptoms associated with a stroke and consists of eleven categories. The PedNIHSS was developed by a panel of pediatric and adult stroke experts and is a modification of the adult NIH stroke scale (NIHSS). Modifications were made to allow individuals age 18 or younger to be assessed and are identified in the PedNIHSS by bold italic text.
For each category of the PedNIHSS, the examiner asks the respondent to perform an activity or respond to an action by the provider. Respondents receive a score for each category based upon their ability to complete the activity or respond to the action. Each score typically ranges from 0 to 3. Each category of the PedNIHSS is designed to determine the respondent’s level of consciousness (LOC), visual, motor, or language ability.
Specific Instructions
The National Institute of Neurological Disorders and Stroke (NINDS) provides a comprehensive interactive training DVD for the NIHSS. Information and purchasing details for this training is available on the NINDS website: www.ninds.nih.gov/doctors/stroke_scale_training.htm.
Availability
This protocol is freely available; permission not required for use.
Protocol
Pediatric NIH Stroke Scale (PedNIHSS)
| Item # and Instructions | Scale Definition and Scoring Guide |
| 1a. Level of Consciousness:the investigator must choose a response, even if a full evaluation is prevented by such obstacles as an endotracheal tube, language barrier, orotracheal trauma/bandages. A 3 is scored only if the patient makes no movement (other than reflexive posturing) in response to noxious stimulation. | 0 = Alert; keenly responsive. 1 = Not alert, but arousable by minor stimulation to obey, answer, or respond. 2 = Not alert, requires repeated stimulation to attend, or is obtunded and requires strong or painful stimulation to make movements (not stereotyped). 3 = Responds only with reflex motor or autonomic effects or totally unresponsive, flaccid, areflexic. |
| 1b. LOC Questions: The patient is asked the month and his/her age. The answer must be correct - there is no partial credit for being close. Aphasic and stuporous patients who do not comprehend the questions will score 2. Patients unable to speak because of endotracheal intubation, orotracheal trauma, severe dysarthria from any cause, language barrier or any other problem not secondary to aphasia are given a 1. It is important that only the initial answer be graded and that the examiner not "help" the patient with verbal or non-verbal cues. Modified for children,age 2 years and up. A familiar Family Member must be present for this item: Ask the child "how old are you?" Or "How many years old are you?" for question number one. Give credit if the child states the correct age, or shows the correct number of fingers for his/her age. For the second question, ask the child "where is XX?", XX referring to the name of the parent or other familiar family member present. Use the name for that person which the child typically uses, e.g. "mommy". Give credit if the child correctly points to or gazes purposefully in the direction of the family member. | 0 = Answers both questions correctly. 1 = Answers one question correctly. 2 = Answers neither question correctly. |
| 1c. LOC Commands:The patient is asked to open and close the eyes and then to grip and release the non-paretic hand. For children one may substitute the command to grip the hand with the command "show me your nose" or "touch your nose". Substitute another one step command if the hands cannot be used. Credit is given if an unequivocal attempt is made but not completed due to weakness. If the patient does not respond to command, the task should be demonstrated to them (pantomime) and score the result (i.e., follows none, one or two commands). Patients with trauma, amputation, or other physical impediments should be given suitable one-step commands. Only the first attempt is scored. | 0 = Performs both tasks correctly 1 = Performs one task correctly 2 = Performs neither task correctly |
| 2. Best Gaze:Only horizontal eye movements will be tested. Voluntary or reflexive (oculocephalic) eye movements will be scored but caloric testing is not done. If the patient has a conjugate deviation of the eyes that can be overcome by voluntary or reflexive activity, the score will be 1. If a patient has an isolated peripheral nerve paresis (CN III, IV or VI) score a 1. Gaze is testable in all aphasic patients. Patients with ocular trauma, bandages, pre-existing blindness or other disorder of visual acuity or fields should be tested with reflexive movements and a choice made by the investigator. Establishing eye contact and then moving about the patient from side to side will occasionally clarify the presence of a partial gaze palsy. | 0 = Normal 1 = Partial gaze palsy. This score is given when gaze is abnormal in one or both eyes, but where forced deviation or total gaze paresis are not present. 2 = Forced deviation, or total gaze paresis not overcome by the oculocephalic maneuver. |
| 3. Visual:Visual fields (upper and lower quadrants) are tested by confrontation, using finger counting (for children > 6 years) or visual threat (for children age 2 to 6 years) as appropriate. Patient must be encouraged, but if they look at the side of the moving fingers appropriately, this can be scored as normal. If there is unilateral blindness or enucleation, visual fields in the remaining eye are scored. Score 1 only if a clear-cut asymmetry, including quadrantanopia is found. If patient is blind from any cause score 3. Double simultaneous stimulation is performed at this point. If there is extinction patient receives a 1 and the results are used to answer question 11. | 0 = No visual loss 1 = Partial hemianopia 2 = Complete hemianopia 3 = Bilateral hemianopia (blind including cortical blindness) |
| 4. Facial Palsy:Ask, or use pantomime to encourage the patient to show teeth or raise eyebrows and close eyes. Score symmetry of grimace in response to noxious stimuli in the poorly responsive or non-comprehending patient. If facial trauma/bandages, orotracheal tube, tape or other physical barrier obscures the face, these should be removed to the extent possible. | 0 = Normal symmetrical movement 1 = Minor paralysis (flattened nasolabial fold, asymmetry on smiling) 2 = Partial paralysis (total or near total paralysis of lower face) 3 = Complete paralysis of one or both sides (absence of facial movement in the upper and lower face) |
| 5 & 6. Motor Arm and Leg: The limb is placed in the appropriate position: extend the arms (palms down) 90 degrees (if sitting) or 45 degrees (if supine) and the leg 30 degrees (always tested supine). Drift is scored if the arm falls before 10 seconds or the leg before 5 seconds. For children too immature to follow precise directions or uncooperative for any reason, power in each limb should be graded by observation of spontaneous or elicited movement according to the same grading scheme, excluding the time limits. The aphasic patient is encouraged using urgency in the voice and pantomime but not noxious stimulation. Each limb is tested in turn, beginning with the non-paretic arm. Only in the case of amputation or joint fusion at the shoulder or hip, or immobilization by an IV board, may the score be "9" and the examiner must clearly write the explanation for scoring as a "9". Score each limb separately. | 5a. Left Arm 5b. Right Arm 0 = No drift, limb holds 90 (or 45) degrees for full 10 seconds. 1 = Drift, Limb holds 90 (or 45) degrees, but drifts down before full 10 seconds; does not hit bed or other support. 2 = Some effort against gravity, limb cannot get to or maintain (if cued) 90 (or 45) degrees, drifts down to bed, but has some effort against gravity. 3 = No effort against gravity, limb falls. 4 = No movement 9 = Amputation, joint fusion explain: |
| 6a. Left Leg 6b. Right Leg 0 = No drift, leg holds 30 degrees position for full 5 seconds. 1 = Drift, leg falls by the end of the 5 second period but does not hit bed. 2 = Some effort against gravity; leg falls to bed by 5 seconds, but has some effort against gravity. 3 = No effort against gravity, leg falls to bed immediately. 4 = No movement 9 = Amputation, joint fusion explain: | |
| 7. Limb Ataxia:This item is aimed at finding evidence of a unilateral cerebellar lesion. Test with eyes open. In case of visual defect, insure testing is done in intact visual field. The finger-nose-finger and heel-shin tests are performed on both sides, and ataxia is scored only if present out of proportion to weakness. In children, substitute this task with reaching for a toy for the upper extremity, and kicking a toy or the examiner’s hand, in children too young (< 5 years) or otherwise uncooperative for the standard exam item. Ataxia is absent in the patient who cannot understand or is paralyzed. Only in the case of amputation or joint fusion may the item be scored "9", and the examiner must clearly write the explanation for not scoring. In case of blindness test by touching nose from extended arm position. | 0 = Absent 1 = Present in one limb 2 = Present in two limbs |
| 8. Sensory:Sensation or grimace to pin prick when tested, or withdrawal from noxious stimulus in the obtunded or aphasic patient. For children too young or otherwise uncooperative for reporting gradations of sensory loss, observe for any behavioral response to pin prick, and score it according to the same scoring scheme as a "normal" response, "mildly diminished" or "severely diminished" response. Only sensory loss attributed to stroke is scored as abnormal and the examiner should test as many body areas [arms (not hands), legs, trunk, face] as needed to accurately check for hemisensory loss. A score of 2, "severe or total," should only be given when a severe or total loss of sensation can be clearly demonstrated. Stuporous and aphasic patients will therefore probably score 1 or 0. | 0 = Normal; no sensory loss. 1 = Mild to moderate sensory loss; patient feels pinprick is less sharp or is dull on the affected side; or there is a loss of superficial pain with pinprick but patient is aware he/she is being touched. 2 = Severe to total sensory loss; patient is not aware of being touched in the face, arm, and leg. |
| 9. Best Language: A great deal of information about comprehension will be obtained during the preceding sections of the examination. For children age 6 years and up with normal language development before onset of stroke: The patient is asked to describe what is happening in the attached picture , to name the items on the attached naming sheet, to repeat words from the attached list, and to read from the attached list of sentences (Table S1; Fig S1, S2, S3). Comprehension is judged from responses here as well as to all of the commands in the preceding general neurological exam. If visual loss interferes with the tests, ask the patient to identify objects placed in the hand, repeat, and produce speech. The intubated patient should be asked to write. The patient in coma (question 1a=3) will arbitrarily score 3 on this item. The examiner must choose a score in the patient with stupor or limited cooperation but a score of 3 should be used only if the patient is mute and follows no one step commands. For children age 2 yrs to 6 yrs (or older children with premorbid language skills < 6 yr level), score this item based on observations of language comprehension and speech during the examination. The patient with brain stem stroke who has bilateral loss of sensation is scored 2. If the patient does not respond and is quadriplegic score 2. Patients in coma (item 1a=3) are arbitrarily given a 2 on this item. | 0 = No aphasia, normal 1 = Mild to moderate aphasia; some obvious loss of fluency or facility of comprehension, without significant limitation on ideas expressed or form of expression. Reduction of speech and/or comprehension, however, makes conversation about provided material difficult or impossible. For example in conversation about provided materials examiner can identify picture or naming card from patient’s response. 2 = Severe aphasia; all communication is through fragmentary expression; great need for inference, questioning, and guessing by the listener. Range of information that can be exchanged is limited; listener carries burden of communication. Examiner cannot identify materials provided from patient response. 3 = Mute, global aphasia; no usable speech or auditory comprehension. |
| 10. Dysarthria:If patient is thought to be normal an adequate sample of speech must be obtained by asking patient to read or repeat words from the attached list. If the patient has severe aphasia, the clarity of articulation of spontaneous speech can be rated. Only if the patient is intubated or has other physical barrier to producing speech, may the item be scored "9", and the examiner must clearly write an explanation for not scoring. Do not tell the patient why he/she is being tested. | 0 = Normal 1 = Mild to moderate; patient slurs at least some words and, at worst, can be understood with some difficulty. 2 = Severe; patient’s speech is so slurred as to be unintelligible in the absence of or out of proportion to any dysphasia, or is mute/anarthric. 9 = Intubated or other physical barrier, explain: |
| 11. Extinction and Inattention (formerly Neglect): Sufficient information to identify neglect may be obtained during the prior testing. If the patient has a severe visual loss preventing visual double simultaneous stimulation, and the cutaneous stimuli are normal, the score is normal. If the patient has aphasia but does appear to attend to both sides, the score is normal. The presence of visual spatial neglect or anosagnosia may also be taken as evidence of abnormality. Since the abnormality is scored only if present, the item is never untestable. | 0 = No abnormality. 1 = Visual, tactile, auditory, spatial, or personal inattention or extinction to bilateral simultaneous stimulation in one of the sensory modalities. 2 = Profound hemi-inattention or hemi-inattention to more than one modality. Does not recognize own hand or orients to only one side of space. |
Table S1. Language testing items for PedNIHSS:
| Repetition | Each of 4 word-repetition tasks is presented: a. Stop b. Stop and go c. If it rains we play inside d. The President lives in Washington |
| Reading | Each of 3 items is presented for the child to read in Fig 1. Adjust expectations according to child’s age/school level |
| Naming | Pictures are presented and of a clock, pencil, skateboard, shirt, baseball, bicycle (Fig 2). |
| Fluency and word finding | The picture (Fig 3) is presented and the child is asked to describe what he/she sees. |
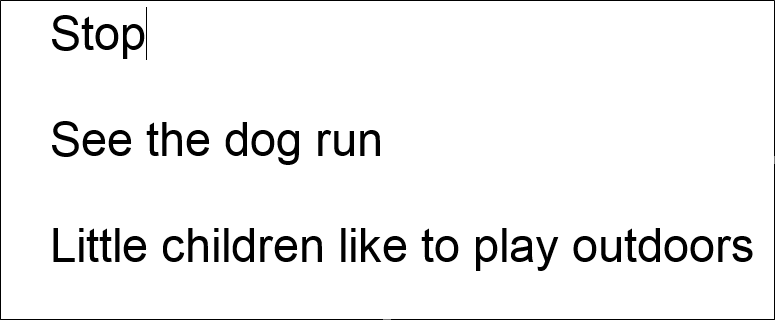
Fig S1. Reading items for PedNIHSS
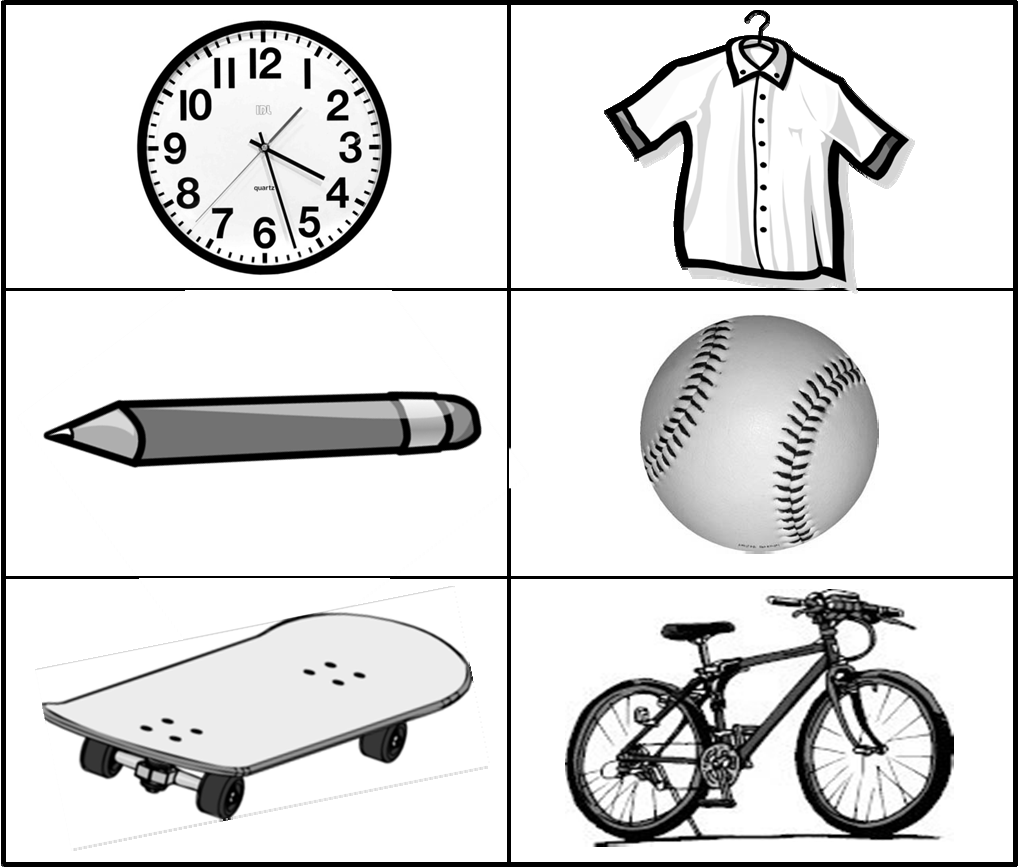
Fig. S2 Pictures to test naming for Item 9 Best Language of PedNIHSS
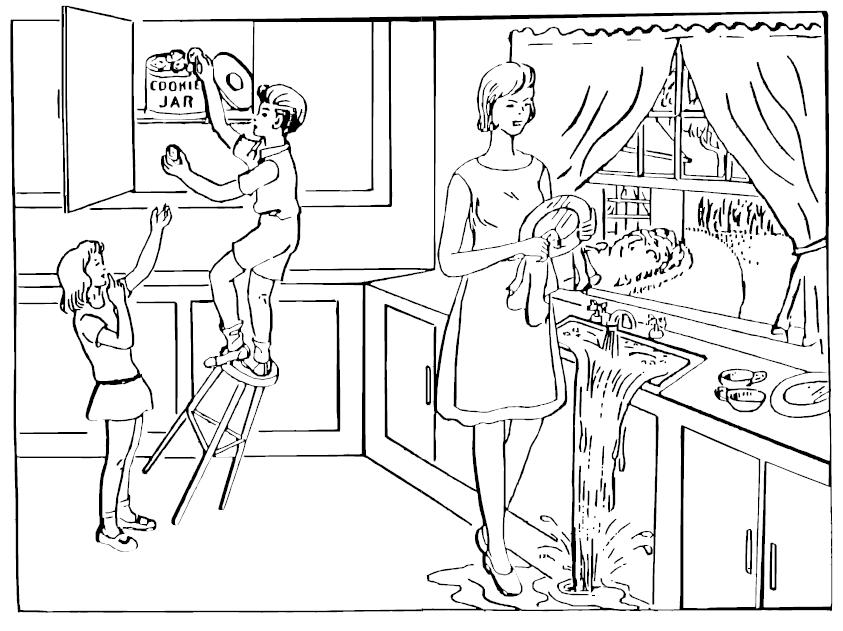
Fig. S3 Picture to test story-telling for Item 9 Best Language of PedNIHSS
Personnel and Training Required
Examiners must be trained to administer, score, and interpret the NIHSS. The National Institute of Neurological Disorders and Stroke (NINDS) provides a comprehensive interactive training DVD for the National Institutes of Health Stroke Scale (NIHSS). Information and purchasing details for this training is available on the NINDS website: www.ninds.nih.gov/doctors/stroke_scale_training.htm
Equipment Needs
None
Requirements
| Requirement Category | Required |
|---|---|
| Major equipment | No |
| Specialized training | No |
| Specialized requirements for biospecimen collection | No |
| Average time of greater than 15 minutes in an unaffected individual | No |
Mode of Administration
Physical Examination
Lifestage
Toddler, Child, Adolescent
Participants
Children and adolescents, ages 2-18 years old.
Selection Rationale
The Sickle Cell Disease Neurology, Quality of Life, and Health Services Working Group selected the Pediatric NIH Stroke Scale (PedNIHSS) because it is a comprehensive, reliable, validated, and widely used evaluation of the effects of a stroke. In addition, scores from the PedNIHSS correlate to infarct size.
The PedNIHSS is a pediatric version of the NIHSS (see Stroke Impact/Outcome-Adults). By using both of these tools, investigators can collect comparable data about stroke in both pediatric and adult populations.
Language
English
Standards
| Standard | Name | ID | Source |
|---|---|---|---|
| Human Phenotype Ontology | Sickle Cell Anemia | ORPHA:232 | HPO |
| Human Phenotype Ontology | Anemia | OMIM:603903 | HPO |
| caDSR Form | PhenX PX820802 - Pediatric Nih Stroke Scale Pednihss | 6254426 | caDSR Form |
Derived Variables
None
Process and Review
Not applicable.
Protocol Name from Source
Pediatric National Institutes of Health Stroke Scale (PedNIHSS)
Source
Ichord, R.N., Bastian, R., Abraham, L., Askalan, R., Benedict, S., Bernard, T.J,, Beslow, L., Deveber, G., Dowling, M., Friedman, N., Fullerton, H., Jordan, L., Kan, L., Kirton, A., Amlie-Lefond, C., Licht, D., Lo, W., McClure, C., Pavlakis, S., Smith, S.E., Tan, M., Kasner, S., & Jawad, A.F. (2011). Interrater reliability of the Pediatric National Institutes of Health Stroke Scale (PedNIHSS) in a multicenter study. Stroke, 42(3), 613-617.
General References
Beslow, L. A., Kasner, S. E., Smith, S. E., Mullen, M. T., Kirschen, M. P., Bastian, R. A., Dowling, M. M., Lo, W., Jordan, L. C., Bernard, T. J., Friedman, N., DeVeber, G., Kirton, A., Abraham, L., Licht, D. J., Jawad, A. F., Ellenberg, J. H., Lautenbach, E., & Ichord, R .N. (2012). Concurrent validity and reliability of retrospective scoring of the Pediatric National Institutes of Health Stroke Scale. Stroke 43(2), 341-345.
Schmülling, S., Grond, M., Rudolf, J., & Kiencke, P. (1998). Training as a prerequisite for reliable use of NIH Stroke Scale. Stroke, 29(6), 1258-1259.
Protocol ID
820802
Variables
Export Variables| Variable Name | Variable ID | Variable Description | dbGaP Mapping | |
|---|---|---|---|---|
| PX820802_StrokeImpactOutcomePediatrics_Best_Gaze | ||||
| PX820802020000 | Best Gaze: Only horizontal eye movements more | N/A | ||
| PX820802_StrokeImpactOutcomePediatrics_Best_Language | ||||
| PX820802090000 | Best Language: A great deal of information more | N/A | ||
| PX820802_StrokeImpactOutcomePediatrics_Dysarthria | ||||
| PX820802100100 | Dysarthria: If patient is thought to be more | N/A | ||
| PX820802_StrokeImpactOutcomePediatrics_Dysarthria_Explain | ||||
| PX820802100200 | Dysarthria: If patient is thought to be more | N/A | ||
| PX820802_StrokeImpactOutcomePediatrics_Extinction_Inattention_Neglect | ||||
| PX820802110000 | Extinction and Inattention (formerly more | N/A | ||
| PX820802_StrokeImpactOutcomePediatrics_Facial_Palsy | ||||
| PX820802040000 | Facial Palsy: Ask, or use pantomime to more | N/A | ||
| PX820802_StrokeImpactOutcomePediatrics_Level_Of_Consciousness | ||||
| PX820802010100 | Level of Consciousness: the investigator more | N/A | ||
| PX820802_StrokeImpactOutcomePediatrics_Limb_Ataxia | ||||
| PX820802070000 | Limb Ataxia: This item is aimed at finding more | N/A | ||
| PX820802_StrokeImpactOutcomePediatrics_LOC_Commands | ||||
| PX820802010300 | LOC Commands: The patient is asked to open more | N/A | ||
| PX820802_StrokeImpactOutcomePediatrics_LOC_Questions | ||||
| PX820802010200 | LOC Questions: The patient is asked the more | N/A | ||
| PX820802_StrokeImpactOutcomePediatrics_Motor_Arm_Left | ||||
| PX820802050101 | Motor Arm and Leg: The limb is placed in the more | N/A | ||
| PX820802_StrokeImpactOutcomePediatrics_Motor_Arm_Left_Explain | ||||
| PX820802050102 | Motor Arm and Leg: The limb is placed in the more | N/A | ||
| PX820802_StrokeImpactOutcomePediatrics_Motor_Arm_Right | ||||
| PX820802050201 | Motor Arm and Leg: The limb is placed in the more | N/A | ||
| PX820802_StrokeImpactOutcomePediatrics_Motor_Arm_Right_Explain | ||||
| PX820802050202 | Motor Arm and Leg: The limb is placed in the more | N/A | ||
| PX820802_StrokeImpactOutcomePediatrics_Motor_Leg_Left | ||||
| PX820802060101 | Motor Arm and Leg: The limb is placed in the more | N/A | ||
| PX820802_StrokeImpactOutcomePediatrics_Motor_Leg_Left_Explain | ||||
| PX820802060102 | Motor Arm and Leg: The limb is placed in the more | N/A | ||
| PX820802_StrokeImpactOutcomePediatrics_Motor_Leg_Right | ||||
| PX820802060201 | Motor Arm and Leg: The limb is placed in the more | N/A | ||
| PX820802_StrokeImpactOutcomePediatrics_Motor_Leg_Right_Explain | ||||
| PX820802060202 | Motor Arm and Leg: The limb is placed in the more | N/A | ||
| PX820802_StrokeImpactOutcomePediatrics_Sensory | ||||
| PX820802080000 | Sensory: Sensation or grimace to pin prick more | N/A | ||
| PX820802_StrokeImpactOutcomePediatrics_Visual | ||||
| PX820802030000 | Visual: Visual fields (upper and lower more | N/A | ||
Measure Name
Stroke Impact/Outcome
Release Date
July 30, 2015
Definition
This measure is a physical assessment to determine neurological deficits due to a stroke.
Purpose
This measure is used to describe the consequences of a stroke and to monitor the effects of treatment and recovery.
Keywords
NIH Stroke Scale, NIHSS, Pediatric NIH Stroke Scale, PedNIHSS, Stroke outcome, stroke, Level of Consciousness, LOC, Visual ability, Motor ability, Language ability, sickle cell disease, SCD, "Neurology, quality of life, and Health Services"
Measure Protocols
| Protocol ID | Protocol Name |
|---|---|
| 820801 | NIH Stroke Scale (NIHSS) |
| 820802 | Pediatric NIH Stroke Scale (PedNIHSS) |